What is GERD?
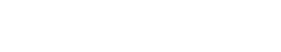
Gastroesophageal reflux disease (GERD) is a chronic condition caused by changes in the gastroesophageal valve (GEV)
that allows acid to flow back from the stomach into the esophagus.
GERD Prevalence and Impact
- GERD is the most common gastrointestinal-related diagnosis made by physicians during clinical visits in the U.S.
- It is estimated that pain and discomfort from acid reflux impacts over 80 million people at least once per month in the U.S.
- GERD can have a significant impact on a patient’s quality of life through persistent typical and atypical symptoms, inconsistent sleep patterns, dietary restrictions, additional health care costs and lost productivity from work.
See http://www.gerdhelp.com/gerd-references/ for more information.
GERD Symptoms
GERD can lead to both typical and atypical bothersome symptoms, which can vary from mild or moderate to severe depending on the individual. These symptoms can include
| Abdominal fullness or bloating Asthma Bad breath Choking while eating or drinking Chronic sore throat Dental erosions or gum disease Difficulty swallowing Discomfort in ears and nose Excessive salivation Excessive throat clearing Feeling of lump in throat Frequent burping | Gas Heartburn and chest pain Laryngitis and hoarseness Persistent dry cough Regurgitation of food or sour liquid Scratchy throat Sensation of food stuck in the throat Shortness of breath Sour or bitter taste in the mouth Sudden coughing episodes Trouble sleeping Wheezing |
Diagnosing GERD
GERD can range in severity and can be a primary condition or a set of symptoms secondary to other chronic gastrointestinal conditions (e.g. nausea, vomiting, inflammatory bowel diseases). Determining the source of typical and/or atypical symptoms is critical to an appropriate treatment plan.
A physician can diagnose GERD based on the presentation of common symptoms, especially in patients with more mild cases. However, the diagnosis of more chronic GERD can be challenging given the variety of symptoms and manifestations.
Some tools a physician may use to diagnose GERD include patient history questionnaires, Esophagogastroduodenoscopy or Endoscopy (EGD), pH monitoring, Impedance, Upper GI Series (Barium Swallow or Esophagram) and Manometry. Optional: insert modality descriptions here
See http://www.gerdhelp.com/gerd-references/ for more information.
Treating GERD
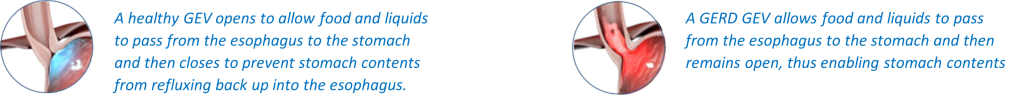
Treatment for GERD varies according to the severity of the symptoms and the individual. The goals of any GERD treatment regimen are symptom control, prevention of GERD-related complications, healing of esophagitis, and to help patients get back to life, free of the distraction and discomfort of GERD. Examples of how GERD can be treated include:
Dietary and lifestyle modifications
Changes in a patient’s diet and lifestyle may help mild GERD sufferers control infrequent symptoms.
Over-the-Counter and Prescribed Medications
Some medicines, such as H2 blockers, antacids, proton pump inhibitors (PPIs), and pro-motility drugs can provide symptom relief, but they do not treat the underlying anatomical problem or stop the disease from progressing. Evidence continues to mount on long-term use of PPIs. Long-term dependency is now associated with complications including negative impacts on the gastrointestinal system, bones, kidneys, heart, nutrient absorption, and shortened lifespan.
Anti-Reflux Surgery
Chronic GERD sufferers may benefit from incisionless interventions and/or laparoscopic surgeries designed to reconstruct the anatomical components of the anti-reflux barrier. This approach restores the body’s normal defense against reflux. Conventional surgery has long been considered an effective solution to treating GERD; however, it frequently introduces negative side-effects such as difficulty swallowing (26%), bloating (36%) and increased flatulence (65%).
See http://www.gerdhelp.com/gerd-references/ for more information.
What is the TIF Procedure for Reflux?
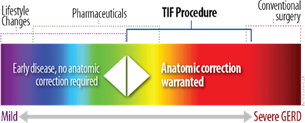
The minimally invasive TIF 2.0 procedure (TIF stands for Transoral Incisionless Fundoplication) is designed to reposition and reconstruct a durable anti-reflux valve while also tightening the Lower Esophageal Sphincter (LES) to restore the body’s natural protection against reflux. It is performed endoscopically through the mouth, meaning there are no incisions necessary.
Abdominal incisions are not required unless additional treatments are being performed with the TIF procedure, such as a hiatal hernia repair (HHR). For patients presenting with both GERD and a hiatal hernia measuring >2cm, a laparoscopic or robotic hiatal hernia repair may be performed immediately prior to the endoscopic TIF procedure. The HHR plus TIF procedure can be performed in the same anesthesia setting should patient anatomy dictate repair of both a hernia and the antireflux valve.
TIF patients often experience a faster recovery since there is no internal cutting, and clinical studies demonstrate they rarely experience long-term side effects commonly associated with traditional antireflux surgery such as trouble swallowing (dysphagia), gas bloat syndrome and increased flatulence.
To date, the TIF 2.0 procedure has been performed in more than 35,000 patients worldwide. Due to the unique approach of the TIF 2.0 procedure, most patients return to work and normal activities within a few days after the procedure, allowing them to get back to life sooner, free of the distraction and discomfort of GERD.
While the TIF 2.0 procedure has an excellent safety profile and is less invasive than traditional laparoscopic fundoplication, it is important to note that it is still a surgical approach. There are potential risks and complications with any surgery, including those with an endoscopic approach, which can include but are not limited to sore throat, musculoskeletal pain, epigastric or abdominal pain and difficulty swallowing.
See http://www.gerdhelp.com/gerd-references/ for more information.